An international study on cost of not breastfeeding estimates that in India inadequate breastfeeding results in 100,000 preventable child deaths (mainly due to diarrhoea and pneumonia), 34.7million cases of diarrhoea, 2.4 million cases of pneumonia, and 40,382 cases of obesity in India. Health impact on mothers is more than 7000 cases of breast cancer, 1700 of ovarian cancer and 87000 of type- 2 diabetes and India spends INR 727.18 crores on health care due to illness. Optimal feeding has the potential to simultaneously reduce the risk or burden of under-nutrition and overweight, obesityor diet-related NCDs (including type 2 diabetes, cardiovascular disease and some cancers). Review of the global evidence reveals that implementing BFHI/Ten Steps is beneficial to enhance early and exclusive breastfeeding (Pérez-Escamilla et al 2016).
Despite the unparalleled value, the breastfeeding rates remain low in India. The NFHS-5, National data revealed that 88.6% women deliver in hospitals, 41.8% are able to begin breastfeeding within an hour of birth, 63.7% breastfed exclusively during 0-6 months,45.9 % received timely complementary feeds at 6-8 months and only 11.1% received adequate diet during 6-23 months..
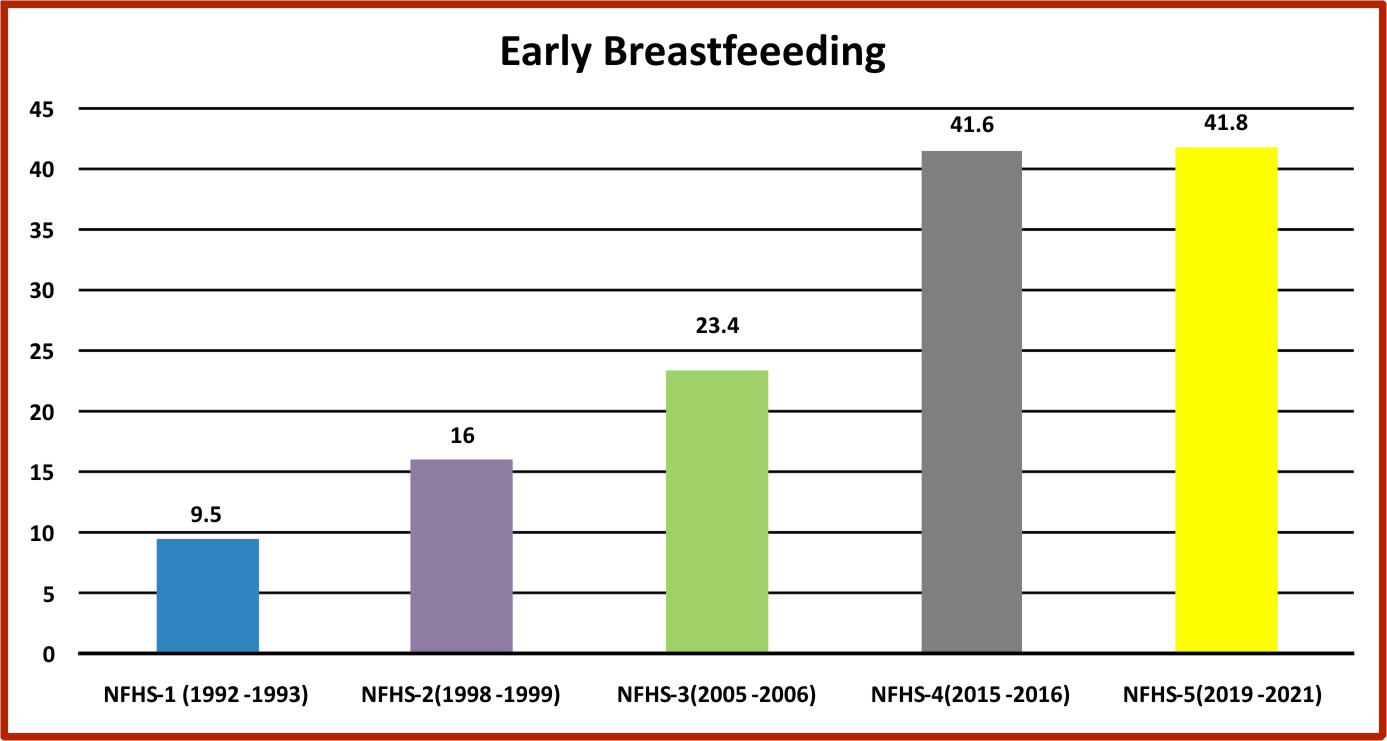
Initiation of breastfeeding within one hour of birth has increased from 9.5% in NFHS-1(1992-93) to 41.8 % in NFHS – 5 (2015-16) However, in 18 states and Union Territories, the rate of early breastfeeding has declined compared to NFHS-4 data (2015-16). Comparing NFHS-4 and NFHS-5 early breastfeeding rate is almost stagnant, which is a matter of concern. This is key are of BFHI-India NAC.
Exclusive breastfeeding in infants <6 months of age has increased from 54.9% in NFHS-4 to 63.7 % in NFHS-5. Pre-lacteal feeding has gone down from 57.2% in NFHS-3 to 21.1% NFHS-4. In some states of India, it remains very high, e.g., in Uttar Pradesh 41.5% and in Uttarakhand 39.1%. One of the worrisome trends is an increasing use of bottle-feeding. According to NFHS-4, every fifth infant (6-9 months) in India is being bottle-fed. Analysis of breastfeeding and progress towards SDGs underlines the need for concrete action to improve breastfeeding rates in health facilities.
In view of majorityof births happening in the health facilities, there is huge scope for improvement in the practice of early initiation of breastfeeding. According to a recent qualitative World Bank Study on BFHI in the South Asia region, including India, BFHI does not receive the attention it needs. Challenges reported from India include: “(a) lack of ownership and funding of BFHI, (b) inadequate human resources, (c) over burdened health facilities, (d) weak monitoring and evaluation mechanisms, (e) inability to involve private hospitals, (f) ineffective implementation of the International Code of Marketing of Breastmilk Substitutes (the Code) and (g) lack of proper mechanisms to provide technical support and leadership. At the hospital level, separation of babies from mothers especially in cesarean section births, more so in the private sector; inadequately trained health staff; unnecessary use of infant formula due to commercial influence of baby food industry on health facilities; and inadequate counselling and support to mothers during antenatal and postnatal periods were some additional barriers to success of BFHI implementation”.
The MAA programme guidance and the WHO guidance with the revised “Ten Steps to Successful Breastfeeding” urge hospitals to follow some policies and practices, like e.g. implementing the Infant Milk Substitutes Feeding Bottles and Infant Foods (Regulation of Production, Supply and Distribution) Act 1992, and Amendment Act 2003 (IMSAct), written feeding policy, data management system, competent staff by training of staff in breastfeeding counselling, antenatal counselling on breastfeeding, support at birth to initiate breastfeeding, breastfeeding friendly practices like rooming-in, avoiding foods other than breastmilk unless medically indicated etc. The World Bank study recommends couple of actions at national level and state level. The one at national level includes coordinated technical support for lactation counselling and periodic monitoring, and external assessment of health facilities at least every five years.
As per the guidance of the MAA programme of Government of India a pool of assessors would be created at State/District level, under the oversight of National Accreditation Centre (NAC). The assessors would be qualified personnel, trained and willing to carryout assessment of health facilities in the private sector. The NAC will maintain the state wise list of assessors who have been authorised for this work
With this background, BPNI and AHPI jointly launch the National Accreditation Centre to accelerate implementation of Ten Steps to Successful Breastfeeding in the private hospitals.